Natalie L. Marks, DVM, CVJ, CCFP, Elite FFCP-V
While our profession originated in preventive medicine, many veterinarians today spend most of their time on chronic disease detection and management. Some of this shift is due to cats living inside the home with longer lifespans. However, other significant factors include pet parents waiting longer to seek veterinary care due to myths about cat health and the rising costs of veterinary medicine.
As Fear Free Certified Professionals, we don’t just consider physical health but also the emotional health of the feline patient, pet parent, and our teams. When specifically thinking about how this applies to the diagnosis and management of our feline diabetic patients, there are two fundamental tenets for success: educating cat caregivers on signs of diabetes for earlier detection and offering alternative treatment options for qualifying patients to ensure complete health.
With a diagnosis of diabetes, some colleagues may question why we need another treatment besides insulin. For one, owner compliance with needles, insulin administration, and insulin overdosing are of concern. Also, we know that there is an increasing number of cats being diagnosed with diabetes. An estimated 600,000 cats in the U.S. are diagnosed with diabetes during their lifetime, with the prevalence of this devastating disease increasing over the past decade. However, the most crucial statistic from research shows that 125,000 cats go untreated1.
Early Detection
We must continue to educate pet parents about the more common signs of diabetes. Urban myths circulate with inaccurate information, such as the idea that indoor cats don’t need routine veterinary care and that these cats vocalize when they don’t feel well.
Instead of acquiescing, let’s provide simple early-detection guidelines. Here are the four most common signs of feline diabetics displayed through the mnemonic “MEOW:”
- More eating and drinking
- Excessive appetite
- Overweight
- Weight loss that occurs suddenly
This can be used in several social media posts—be sure to communicate this to pet parents where they can best receive information!
In addition to the most common signs, it’s also helpful to give pet parents an idea of other risks. Some of the increased risk factors for dogs hold for cats, like chronic pancreatitis, being middle age, and use of steroids, but there are definite differences
that your cat’s parents want to know! This is especially true with how much of a role obesity plays – cats with an obese body condition score are four times more likely to develop diabetes! Besides the other complications of obesity, this is a big reason to ALWAYS give our patients a body condition score and discuss appropriate weight management guidelines. Indoor cats, neutered males, chronic kidney cats, and hyperthyroid kitties are also at risk.
When pet parents call for an appointment based on the clinical signs observed at home, continuing the education process during the physical exam is essential. Cats are very similar in pathophysiology to overweight adults; 80% (or more)2 have Type 2 diabetes. This is due to either an insensitivity or resistance to insulin in tissues. Pancreatic beta cells don’t like a high glucose environment or being overtaxed. When that happens, we see the progressive loss of beta-cell insulin production and burnout.
Diagnosis of diabetes also requires diagnostics. Let’s recommend a foundational diagnostic workup instead of just a blood glucose spot check. This includes a full CBC (complete blood count), a chemistry panel with electrolytes, a concurrent urinalysis with culture (preferably low colony count), a UPC (urine protein: creatinine ratio), blood pressure, and a thyroid panel. While many of our patients develop their diabetic state secondary to adipocyte inflammation, we can see other associated disease states like chronic kidney disease, hypertension, hyperthyroidism, and acromegaly.
Fear Free Treatment Options
Insulin is a successful treatment option for many diabetic cats. However, a large population remains completely untreated, and for those yet to be diagnosed, insulin may not be a good fit for the family’s lifestyle. Veterinary teams must provide safe and effective treatment alternatives.
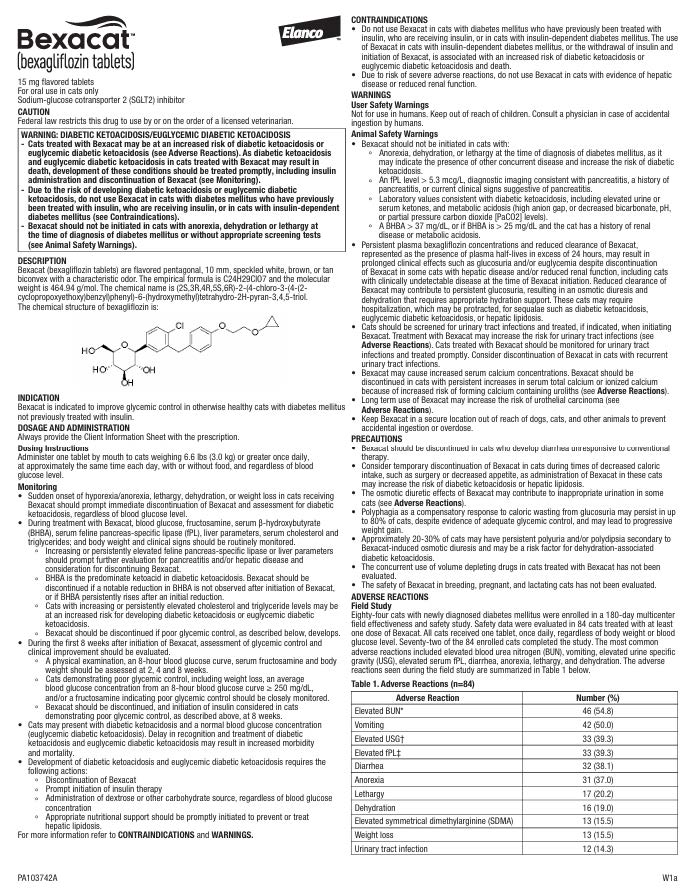
Bexacat™ (bexagliflozin tablets) is the first sodium-glucose cotransporter 2 (SGLT2) inhibitor approved by the FDA in any animal species. Bexacat™ introduces a mechanism of action for veterinarians and pet owners that offers a non-insulin, needle-free, once-daily oral medication specifically designed for cats with diabetes mellitus. This first-in-class therapeutic is indicated to improve glycemic control in otherwise healthy cats with diabetes mellitus NOT previously treated with insulin.
Let’s consider what’s different about the mechanism of Bexacat™ vs. traditional insulin. Insulin drives glucose into the cells, whereas Bexacat™ drops blood glucose levels by promoting urinary excretion or preventing renal glucose reabsorption.
Several differentiating features of Bexacat™ help promote physical and emotional health. First, unlike traditional insulin, Bexacat™ does not require dosing calculations or titration, measuring in syringes, or potential dosing errors. It’s one flavored tablet per cat daily and can be given in food. Not only does this streamline the process for clients, but it also helps them efficiently manage their schedules or travel demands by
having other caregivers participate. The tablet has been shown to have 96-97% palatability in studies3, which also encourages easing client compliance!
Another unique characteristic of Bexacat™ is that dosing is independent of our patient’s blood sugar or if the cat gains or loses weight. This is incredibly helpful in easing the minds of cat parents, especially as we start to talk about the possibility of remission monitoring. We need a minimum weight of 3kg for cats taking Bexacat™.
The essential piece of success is case selection. At this point, Type 1 Diabetics and feline patients who have been on traditional insulin are not candidates for Bexacat™ use. This is because when cats have been diabetics for a long time or are Type 1 (insulin-dependent), they don’t have enough healthy B-cells in their pancreas to produce insulin – an essential qualification to use Bexacat™. The longer a cat has diabetes mellitus, the higher the risk of amyloidosis and beta cell depletion. A newly diagnosed cat will likely have a larger beta cell mass and be more likely to be able to produce at least some insulin. Cats also need to be able to secrete endogenous insulin. However, no accurate test exists to determine this. Glucose toxicity from hyperglycemia is toxic to beta cells.
Finally, patients also need qualifying lab work. Any significant renal (Stage III IRIS or higher) or significant hepatic disease disqualifies the patient. We also need to rule out DKA (diabetic ketoacidosis). But, the final piece, and what may be very new to many of us, is a beta-hydroxbutyrate (BHBA) level of <37 mg/dL or 3.6 mmol/L and precaution of <25 mg.dl or 2.4 mmol/L if history of renal disease or metabolic acidosis. We can use a BHBA level of 2.4 mmol/L if using a handheld monitor. If ketones are in the urine, exclude the cat from being a good candidate.
References:
- https://www.businesswire.com/news/home/20221209005431/en/Elanco-Announces-FDA-Approval-of-Bexacat%E2%84%A2-bexagliflozin-tablets-%E2%80%93-the-First-of-its-Kind-Oral-Feline-Diabetes-Treatment-Option
- Chandler M, Cunningham S, Lund EM, Khanna C, Naramore R, Patel A, Day MJ. Obesity and Associated Comorbidities in People and Companion Animals: A One Health Perspective. J Comp Pathol. 2017 May;156(4):296-309.
- Elanco Animal Health. Data on File.
Important Safety Information:
Before using Bexacat, you must read the entire package insert, including the boxed warning. Cats treated with Bexacat may be at an increased risk for conditions called diabetic ketoacidosis or euglycemic diabetic ketoacidosis, both of which may result in death. It is critical that cats taking Bexacat be examined by a veterinarian promptly if sudden decreases in appetite or water consumption occur, or if weight loss, tiredness, vomiting, diarrhea, or weakness are seen. Discontinue Bexacat and call your veterinarian immediately if any of these occur as they could be signs of diabetic ketoacidosis or
euglycemic diabetic ketoacidosis. Before giving Bexacat, be sure to talk with your veterinarian about any past illnesses your cat has had including if your cat has ever been on insulin, as cats that have been treated with insulin should not receive Bexacat. Do not use Bexacat if your cat has experienced pancreatitis, liver disease or reduced kidney function as serious side effects may occur. Bexacat is available by veterinary prescription only. Not for human use. Keep out of reach of children. Contact a physician immediately if swallowed accidentally.
Bexacat, Elanco and the diagonal bar logo are trademarks of Elanco or its affiliates.
©2024 Elanco or its affiliates. PM-US-24-0954
This article was reviewed/edited by board-certified veterinary behaviorist Dr. Kenneth Martin and/or veterinary technician specialist in behavior Debbie Martin, LVT.
Want to learn more about Fear Free? Sign up for our newsletter to stay in the loop on upcoming events, specials, courses, and more by clicking here.




